Introduction
Testosterone is a steroid hormone that plays a crucial role in various bodily functions, from muscle growth to cognitive health. It is essential for both men and women, but it’s often associated with masculinity and male characteristics. This series of articles delves into the world of testosterone, its functions, regulation, and the controversies surrounding testosterone replacement therapy (TRT).
The Basics of Testosterone
Testosterone is a steroid hormone derived from the cholesterol family, synthesized through a series of steps. This synthesis typically occurs in the Leydig cells of the testes in men and in smaller quantities in women’s ovaries and adrenal glands. Its effects are primarily mediated by binding to an androgen receptor, located outside the cell nucleus. Unlike molecules such as glucose or electrolytes, testosterone is hydrophobic, allowing it to easily penetrate cell membranes without requiring specialized channels or receptors.
Carrier Proteins for Testosterone
To travel through the bloodstream, testosterone needs carrier proteins, similar to how cholesterol requires lipoproteins. Two dominant carrier proteins for testosterone are Sex Hormone-Binding Globulin (SHBG) and albumin. SHBG is responsible for about two-thirds of testosterone’s carrying capacity, while albumin accounts for the remaining one-third. These proteins transport testosterone in the blood, making it soluble and aiding in its distribution to target tissues.
The Unbound Portion of Testosterone
What’s crucial to understand is that only the unbound portion of testosterone can exert biological influence. This unbound fraction is often referred to as “free testosterone.” It’s the active form of testosterone that can readily interact with androgen receptors on cells. Bioavailable testosterone includes the tiny fraction that is completely unbound, as well as the larger fraction bound to albumin. From a clinical perspective, symptoms typically track more closely with free testosterone than with bioavailable testosterone.
How Testosterone Functions in the Body
Testosterone enters cells and binds to androgen receptors, leading to a conformational change in the receptor. This change initiates a cascade of intracellular events that ultimately affect gene transcription. Heat shock proteins are displaced, and dimerization occurs, meaning two androgen receptor molecules combine. This dimer then translocates into the cell nucleus, where it binds to a hormone response element, directly affecting the expression of various genes. Testosterone plays a vital role in regulating anabolic and growth-related characteristics in the body, such as muscle development and bone density.
Dihydrotestosterone (DHT): A Potent Form of Testosterone
Dihydrotestosterone (DHT) is a derivative of testosterone that is three to six times more potent in binding to androgen receptors. DHT is synthesized from testosterone by the enzyme 5-alpha reductase, which catalyzes the conversion of testosterone into DHT. DHT plays a crucial role in hair loss and prostate gland hyperplasia. It has a higher affinity for androgen receptors than testosterone and is responsible for the development of secondary sexual characteristics in men.
In the context of hair loss, DHT is known to drive male pattern baldness. It’s also implicated in the growth of the prostate gland, which can lead to benign prostatic hypertrophy (BPH). To address these issues, medications like finasteride are used to inhibit 5-alpha reductase and reduce the conversion of testosterone to DHT.
Regulating Testosterone Levels Naturally
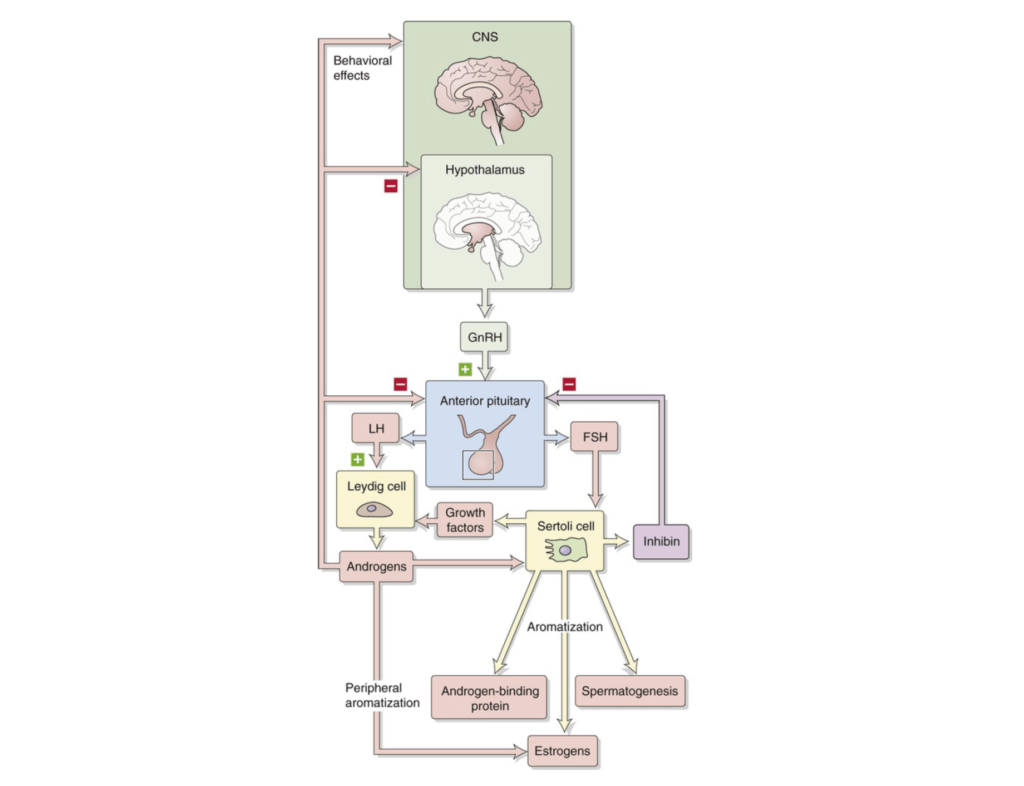
Figure 1. Hypothalamic-pituitary-gonadal axis. (Boron and Boulpaep, 2016).
- There is a feedback loop in this process involving the central nervous system, specifically the hypothalamus. When testosterone levels are low, the hypothalamus secretes gonadotropin-releasing hormone (GnRH). This hormone targets the pituitary gland, which is divided into two parts: the anterior and the posterior.
- In response to GnRH, the anterior pituitary gland releases two hormones that are commonly measured in blood tests:
- Luteinizing hormone (LH)
- Follicle-stimulating hormone (FSH)
- LH and FSH enter the bloodstream and target two types of cells in the testes:
- Sertoli cells
- Leydig cells
- Sertoli cells secrete growth factors that further stimulate Leydig cells, while LH directly acts on Leydig cells. The net result is the production of testosterone.
- Testosterone can be converted into estrogens through a process called aromatization, which uses specific enzymes, resulting in the co-creation of estradiol.
Key Takeaway:
- When testosterone is low, the feedback loop increases the secretion of LH and FSH.
- Conversely, high testosterone levels signal the inhibition of these hormones.
Clinical Implications:
- If someone is supplementing with testosterone, blood tests typically show unmeasurable levels of LH and FSH along with high testosterone.
- Prolonged use of exogenous testosterone can lead to a permanent inability of the body to produce its own testosterone.
- Clinically, high LH and FSH but low testosterone usually indicate a problem in the testes.
- Low testosterone along with low LH and FSH suggests a central issue, such as a malfunction in the hypothalamus or pituitary gland.
- Common causes for this scenario include sleep deprivation and high stress levels, which interfere with the brain’s signaling to the testes.
- Understanding these distinctions is crucial for deciding how to treat low testosterone, as the treatment approach depends on identifying whether the issue is central or testicular.
Defining Low Testosterone and Its Impact
Low testosterone levels can be defined by measuring total testosterone, but free testosterone is often considered more clinically relevant. The prevalence of low testosterone increases with age, with a significant proportion of men experiencing lower levels as they get older. Low testosterone can have various impacts on health, including:
- Reduced Bone Mineral Density: Low testosterone levels are associated with decreased bone density, making individuals more susceptible to osteoporosis.
- Muscle Mass: Testosterone plays a vital role in muscle development and maintenance. Low testosterone levels can lead to muscle loss and decreased strength.
- Muscle Strength: Low testosterone levels can result in decreased muscle strength and physical performance.
- Cognitive Decline: Testosterone has a role in cognitive functions such as memory and spatial abilities. Reduced testosterone levels may contribute to cognitive decline.
- Libido and Sexual Function: Testosterone plays a critical role in sexual desire and erectile function. Low testosterone levels can lead to reduced libido and sexual dysfunction.
- Diabetes: Low testosterone levels are associated with an increased risk of insulin resistance and type 2 diabetes.
- Fat Mass: Low testosterone levels are often linked to an increase in body fat, particularly visceral fat, which can have adverse health effects.
- Triglycerides and Cholesterol: Testosterone can influence lipid profiles, and low levels may contribute to unfavorable changes in triglycerides and cholesterol.
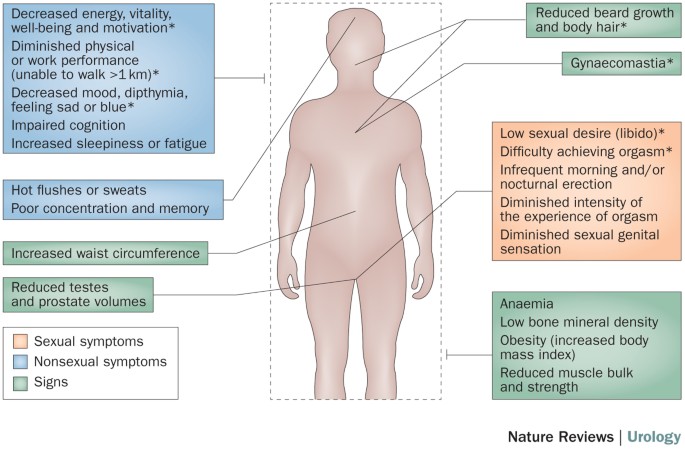
Figure 2. Effects of low testosterone (Aversa, A., Morgentaler, A. The practical management of testosterone deficiency in men. Nat Rev Urol 12, 641–650 (2015). https://doi.org/10.1038/nrurol.2015.238)
It’s important to note that the impact of low testosterone can vary from person to person, and not everyone with low testosterone will experience these effects.
In the next article we will go on to define low testerone and look at how levels decline with age.

