Want to catch up with the other articles in this series?
Part 1: What is the impact of endurance training on human lifespan?
Part 1.1: What is VO2max?
Part 2: What are training zones?
Part 2.1: How do muscle fiber types correspond to training zones?
Part 2.2: Training zones 1, 2 and 3
Part 2.3: Training zones 3, 4, 5 and 6
Part 2.4: Moderate intensity vs. high intensity exercise
Part 3: By which mechanisms does exercise delay aging and prevent chronic disease?
Part 3.1: What are the cardiovascular adaptations to endurance training?
Part 3.2: What are the metabolic adaptations to endurance training?
Part 3.3: Can exercise prevent or even treat cancer?
Part 3.4: How does exercise impact the immune system?
Part 3.5: Exercise as a therapy for neurodegeneration and conclusions
Training zones 1, 2 and 3
Low intensity, or zone 1, represents the minimum contraction on a muscle and is characterised by the use of fat as the primary energy substrate. In training, this would be a recovery day at minimum pace and exertion. For most active people zone 1 would be walking. Sadly, due to declining fitness levels, walking is more often approaching the anaerobic zones for many people.
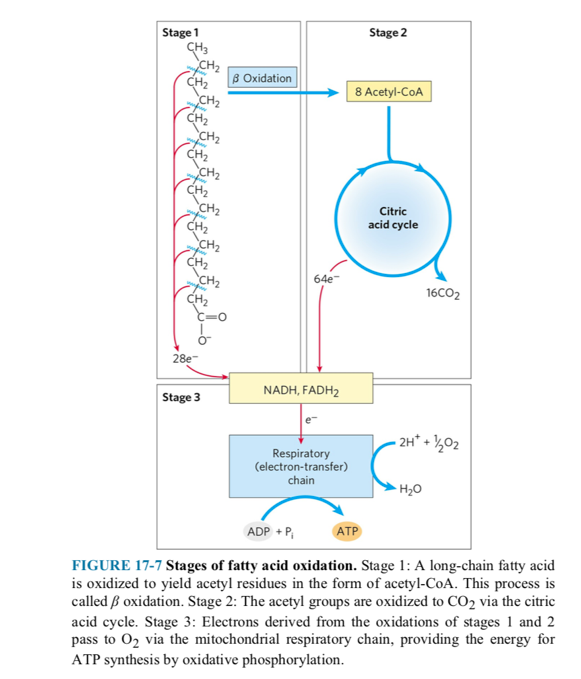
Type I muscle fibers are recruited in zone 1. Type I muscle fibres have a ton of mitochondria (see figure 2). These muscle fibers are rich in blood supply to receive fatty acids from distant fat stores. Because of this apparatus, Type I muscle fibres serve as excellent motor units to oxidise fat into ATP. This occurs in the mitochondria. Humans can store virtually unlimited supplies of fat. Therefore, Type I muscles fibres serve to mobilise us utilising fat without immediate requirement for energy replacement.
Moderate Intensity Continuous Training: Zones 2 & 3
Zone 2
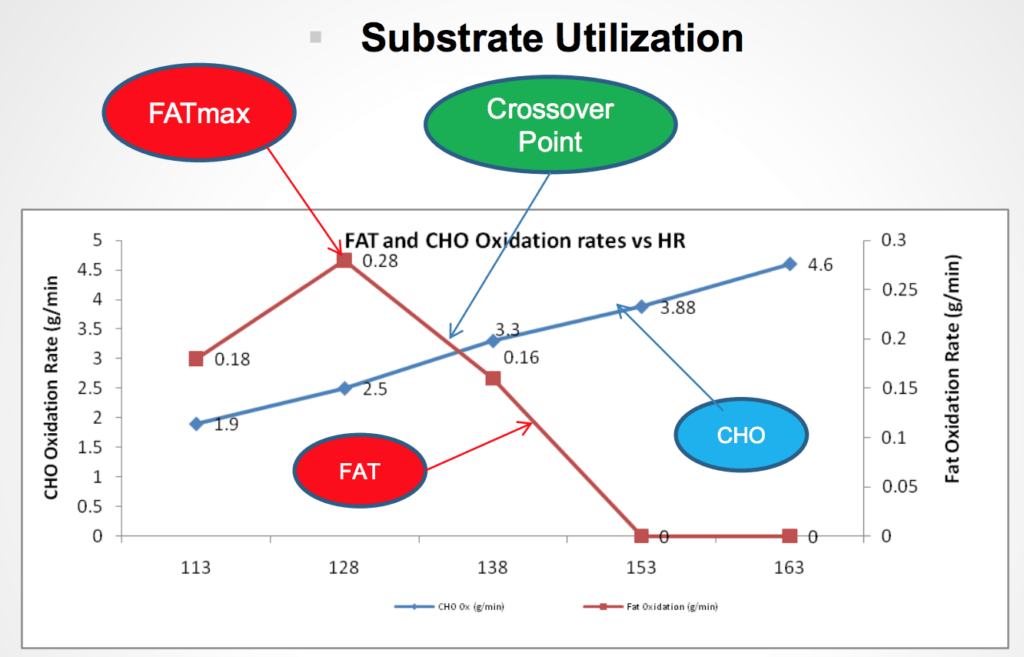
In Zone 2, also known as the “fatmax” zone, the body continues to oxidise fat for energy at the mitochondria. The intensity of exercise is higher than in Zone 1, but still within the range that the body can sustain aerobically.
The maximum rate of fat oxidation occurs at this intensity. This is usually between 60% and 80% of maximum heart rate. It is also known as the “Fatmax Zone” and is within 10% of the actual “Fatmax” intensity (i.e. the maximum amount of fat used to make energy). This type of training is known to be effective for those looking to improve their cardiovascular endurance and maximise the use of stored fat as a fuel source.
Zone 2 is the intensity of exercise athletes generally spend the most time in. In endurance sports such as running or cycling, athletes are spending the majority of their training at this intensity. Kipchoge, widely regarded as the greatest marathon runner of all time, is spending 60-70% of his training around zone 2.
Athletes can perform in zone 2 at extreme levels of output. For example, a fit person’s zone 4 pace would be in an athlete’s zone 2. So, an athlete is on their bike chatting with their training buddy about what they are having for dinner on a ‘coffee ride’ at the same pace I would be at lactate threshold. This demonstrates the importance of individualised training and understanding how we respond to exercise. It also demonstrates the extreme adaptability of the human body in response to training.
Zone 2 is perhaps where the biggest gains in V̇O2 max can be made in increasing VO2max. The beauty of Zone 2 training is that adaptation happens quickly, there appears no ceiling and improving VO2max can have a massive impact on health span. This can’t be understated.
Locating zone 2
There are a variety of parameters that indicate when someone is in zone 2. The gold standard is blood lactate levels— these would remain under 1.8-2 mmol/l.
The rate of perceived exertion would be moderate— we are able to have a conversation while exercising or able to breathe through our nose. Alternatively, we can use roughly 70-80% of our maximum heart rate as an approximation. This is not an exact science. It’s trial and error to find this sweet spot over a prolonged period.
Data shows that the moderately active individual hits 2 mmol lactate at 175 watts but max fat oxidation at 125 watts (see figure 2.5). That’s a 50-watt difference. To improve metabolic function and mitochondrial performance, Zone 2 be defined as somewhere in the middle of 125 -175 watts
For the moderately active individual. This (watts) can easily be tracked on a bike or machine at the gym. Athletes can then extend upon the watt output whilst remaining in this lactate range. As the body becomes adapted athletes can see a watt output of over 300 watts before lactate levels start increasing.
Burning fat as a fuel
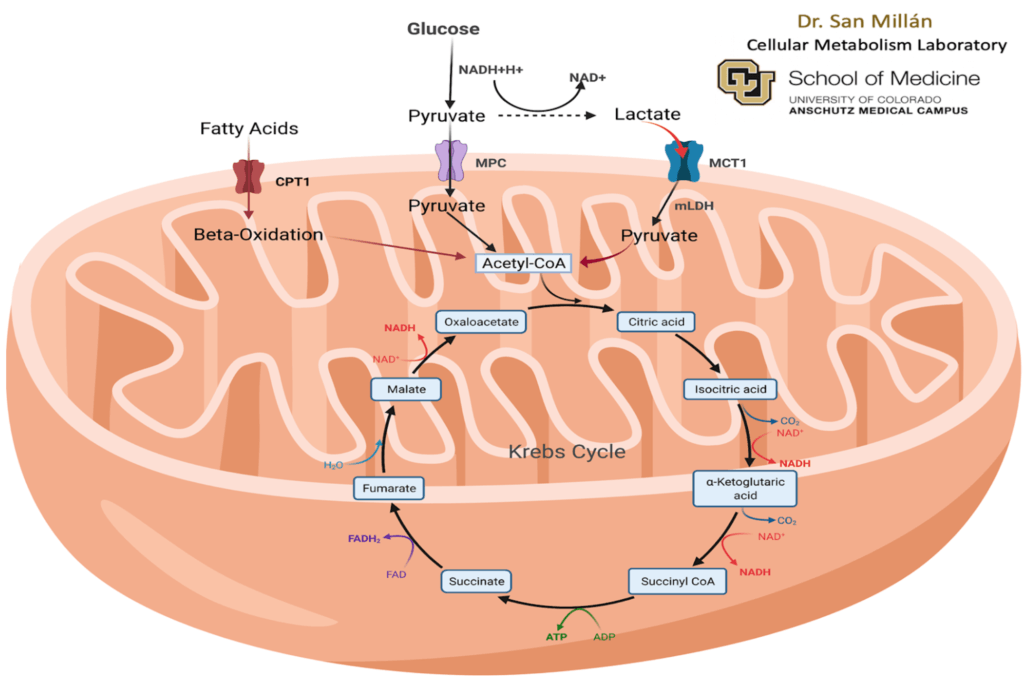
Fatty acid metabolism refers to the series of biochemical reactions that occur within the body to break down and utilise fat for energy. The process begins with the hydrolysis of triglycerides stored in fat cells, releasing free fatty acids into the bloodstream. These fatty acids are then transported via the bloodstream to distant cells throughout the body, where they can be used for energy production.
The biochemical pathways involved in burning fat require many enzymes and reactions, all of which increase in numbers and efficiency as we predominantly rely on fat as a fuel. We can see this in the image below.

Metabolic flexibility
Through zone 2 training, we are looking to improve our cardiorespiratory fitness and become efficient at burning fat. This is a major step in becoming metabolically flexible. Metabolic flexibility refers to the ability to switch between using different energy substrates such as carbohydrates, fats, and ketones as a source of fuel depending on the availability and the body’s needs. Many professional cyclists train in zone 2 so they can they preserve that glycogen for the end of the race to sprint at a very high intensity. This is a fantastic example of metabolic flexibility.
The reason diabetes is so prevalent in developed nations is because many people live in a constant state of energy toxicity. This is when people’s body’s are overwhelmed by the amount of carbs and fat they consume. High energy foods are so abundant and over consumed that many people never even begin to adapt to burning fat. Add on top of this a sedentary lifestyle, most people are actually anabolically building fat through excess energy consumption and barely burning any of their fat stores.
When the body is exposed chronically to fat and carbs, they start depositing fat into their organs leading to loss of function and metabolic disease e.g. diabetes. This is known as visceral fat. This is the definition of being metabolically inflexible. I’ve written in detail about this in my series on diabetes that is on my blog.
By exercising in zone 2 we promote fat utilisation and metabolism, which is extremely important in removing or preventing visceral fat and therefore avoiding many of the prevalent chronic diseases affecting western nations.

Lactate clearance
Besides fat utilisation, type I muscle fibres are also responsible for lactate clearance. Type I muscle fibres (slow twitch fibres) are used for low intensity tasks. As we improve the body’s capacity to utilise type I fibres; they become an optimised organ in utilising and storing fuel.
One of these fuels is ironically lactate. As intensity increases, we begin to utilise anaerobic metabolism in the cytosol of the muscle fiber to produce ATP. Lactate is then produced as a byproduct of glycolysis. In training adapted individuals, lactate can be cleared by type I fibres and recycled as a fuel source. This is how high performing individuals can produce high levels of output while still being in zone 2 (under 2 mmol/l of lactate levels)
In becoming efficient at metabolising both fats and lactate, we’re extending the levels of intensity we can produce, before even entering a predominantly glycolytic energy system. In short, as we become fitter we can put out more power with less effort.
Traditionally we consider lactate a bad thing. However emerging research is identifying lactate as fuel rather than a toxin. It is the blood acidity or H+ that is correlated with rises in lactate that leads to symptoms of extreme fatigue. Lactate is a signalling molecule which our body uses to stop us from exercising at a high intensity for too long.
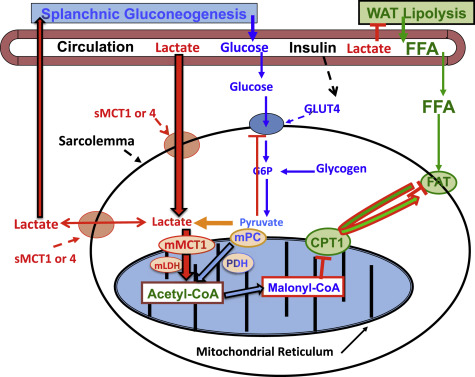
Lactate is the byproduct of glucose metabolism which mainly occurs in fast twitch muscle fibres. A specific transporter called MCT-4, exports lactate from these fibres. Type I muscle fibres play a key role in the clearance of lactate. Type I muscle fibres contain a transporter called MCT-1 which takes up lactate and transports it to the mitochondria where it is reused as energy.
In the figure below, we can see that increased lactate also inhibits lipolysis. What this suggests is that as we crank through the zones and the muscles demand more ATP, lactate acts as a signalling molecule to inhibit the supply of fat to the mitochondria— this corresponds with decreasing fat oxidation and increasing fat blood lactate levels seen in zone 2.
Zone 2 training increases mitochondrial density as well as MCT-1 transporters. By training Zone 2 we will not only improve fat utilisation and preserve glycogen but we will also increase lactate clearance capacity which is key for increasing V̇O2 max.